By the bioMérieux Connection Editors
“[Doctors] make crucial medical decisions—sometimes life or death calls—based on incorrect assumptions that patients have ailments they probably don’t,” says Dr. Daniel Morgan, Associate Professor of Epidemiology, Public Health and Infectious Diseases at the University of Maryland School of Medicine.
Each year, doctors in the U.S. perform more than 4 billion diagnostic tests, which have become more sophisticated and easier to execute as technology has improved. However, research has found that many physicians assume tests are more accurate than they are. For example, the primary blood test to check for a heart attack, known as high-sensitivity troponin, has a 5% false-positive rate. U.S. emergency rooms often administer the test to people with a very low probability of a heart attack and as a result, 84% of positive results are false, according to a study published in 2017.
Misinterpreted false positive tests are one of the many negative outcomes that can come from inappropriate testing. Infectious disease testing in the absence of symptoms often leads to false positive test results, which lead to over-diagnosis and the unnecessary use of antibiotics. Not only can misinterpreted false positives lead to unneeded treatment, but they also increase the odds of putting the patient in danger.
Negative Effects of Inappropriate Testing

The Solution: Diagnostic Stewardship
Diagnostic stewardship can help eliminate inappropriate diagnostic testing and its effects. According to the World Health Organization, “Diagnostic stewardship is defined in the GLASS [Global Antimicrobial Resistance Surveillance System] Manual as: ‘coordinated guidance and interventions to improve appropriate use of microbiological diagnostics to guide therapeutic decisions. It should promote appropriate, timely diagnostic testing, including specimen collection, and pathogen identification and accurate, timely reporting of results to guide patient treatment.’”
GLASS promotes and facilitates standardized antimicrobial resistance (AMR) surveillance worldwide, and the concept of “diagnostic stewardship” at surveillance sites is an important component. The first objective of microbiological diagnostic stewardship is to deliver patient management guided by timely microbiological data to provide safer, more effective, and more efficient patient care. The second objective is to deliver accurate and representative AMR surveillance data to inform treatment guidelines and AMR control strategies.
To spread awareness of diagnostic stewardship and its role in antimicrobial stewardship, in July 2019, bioMérieux launched a webinar series called, “On The Front Lines”, for sharing best practices implemented by hospital antimicrobial stewardship teams. The first webinar was presented by Dr. Victor Leung, MD, FRCPC, the Medical Director of Infection Prevention and Control at Providence Health Care in Vancouver, Canada. A summary of the webinar can be found on bioMérieux Connection. The August webinar will be presented by Dr. Ravina Kullar, PharmD, MPH, FIDSA and a preview is available.
Implementation: Diagnostic Stewardship at Providence Health Care
Providence Health Care helped eliminate unneeded diagnostic tests, as well as the spread of infection and improper antimicrobial use, with diagnostic stewardship. According to Dr. Victor Leung, stewardship work included physician and nurse education, guideline establishment, and coordinated efforts.
Guideline-Driven Approach Leads to Reduced Testing
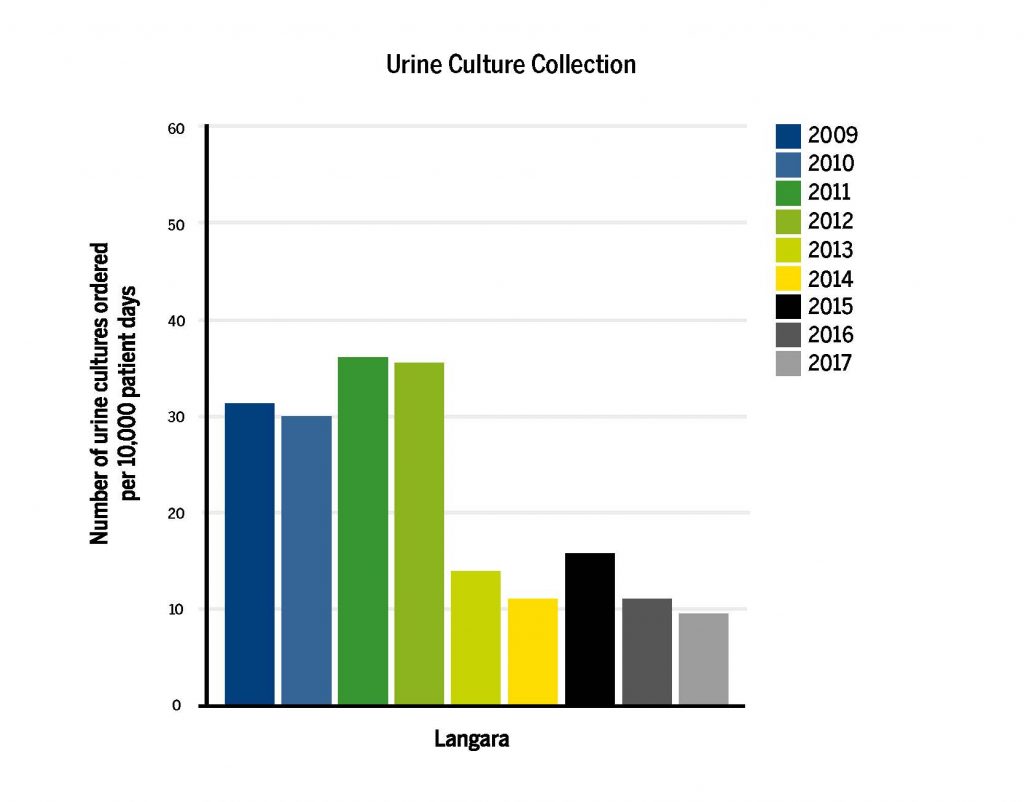
In 2013, Providence Health Care developed a guideline-driven approach to educate long-term care nurses and physicians on UTI symptoms. Overall, the goal was to prevent the collection of unnecessary urine samples. The approach decreased the volume of tests conducted by 50% and also decreased unnecessary antimicrobial use. After implementation, the number of patients needing intensive care for severe infections was unchanged.
To ensure guidelines were met while collecting urine cultures, a checklist method was implemented as a part of the approach. By 2017, Providence Health Care saw a significant decrease in the number of urine cultures collected.
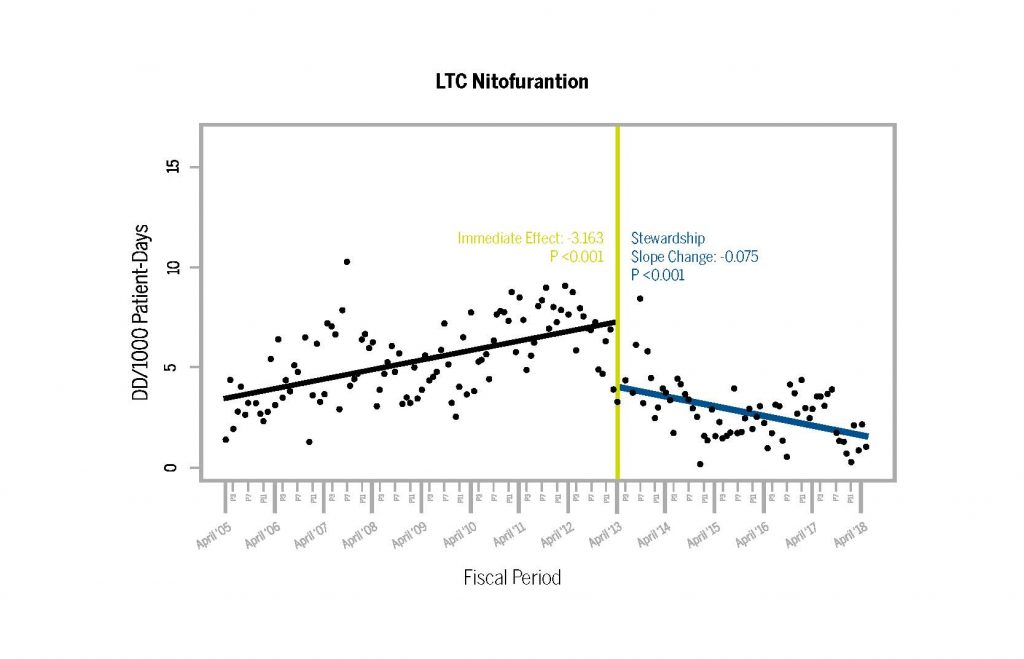
At the same time, the rate of antibiotic use also decreased. Less LTC Nitofurantion, the antibiotic often used to treat UTI’s in long term care facilities, was prescribed after the guideline implementation.
Optimal Testing, Treatment, Prevention, and Control Leads to Reduced C. difficile Infection
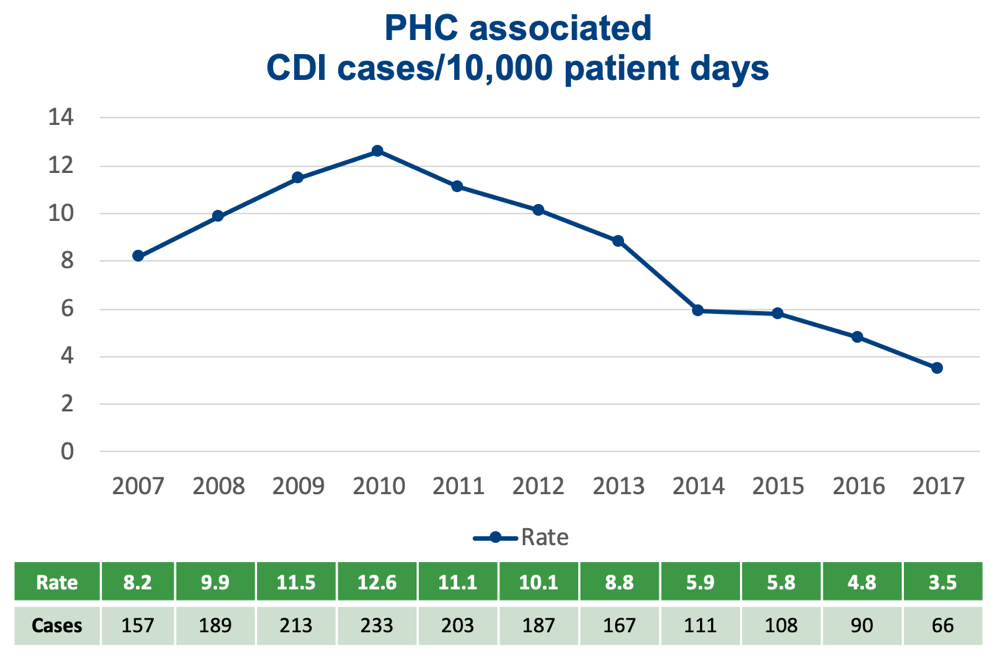
In 2012, Providence Health Care implemented the “War on Spore”. The coordination effort was developed to optimize C. difficile testing and treatment as well as prevent and control C. difficile infections.
The “War on Spore” included the work of the Antimicrobial Stewardship Program and the work of the Infection Prevention and Control team. The health system’s Antimicrobial Stewardship Program helped to determine whether or not testing for C. difficile was needed on a case by case basis, and if so, whether or not antibiotic treatment was necessary. After an infection was found, the health system’s Infection Prevention and Control Team coordinated notification, precaution, cleaning, and education efforts. “The War on Spore” proved to reduce overall infection rates of C. difficile.
At Providence Health Care, unnecessary diagnostic testing and many of its harmful effects were reduced with diagnostic stewardship. Stewardship work included education, guideline establishment, and coordinated efforts. Following 2012-13, the health system was able to perform fewer unnecessary diagnostic tests, prescribe fewer unnecessary antibiotics, and prevent a greater number of infections from spreading. Full elaboration of the diagnostic stewardship efforts and research can be found in the on-demand version of Dr. Victor Leung’s Webinar, Diagnostic Stewardship is a Key Driver of Antimicrobial Use. Registration for future webinars can be completed on bioMérieux’s ASP Webinar page.
Opinions expressed in this article are not necessarily those of bioMérieux, Inc.



